Candidiasis-Atypical Presentation in an Immunocompromised Patient: A Case Report
Srikar Vulugundam1,2 and Aparnaa Upadhyaya1,2*
1Dental Department, Erlanger Health System, Chattanooga, U. S. A .
2Department of restorative dentistry, UTHSC school of Dentistry, Memphis, U. S. A .
Corresponding author Email: srikar.vulugundam@gmail.com
DOI: http://dx.doi.org/10.12944/EDJ.05.01.06
Copy the following to cite this article:
Vulugundam S, Upadhyaya A. Candidiasis – Atypical Presentation in an Immunocompromised Patient: A Case Report. Enviro Dental Journal 2023; 5(1). DOI:http://dx.doi.org/10.12944/EDJ.05.01.06
Copy the following to cite this URL:
Vulugundam S, Upadhyaya A. Candidiasis – Atypical Presentation in an Immunocompromised Patient: A Case Report. Enviro Dental Journal 2023; 5(1).Available here:https://bit.ly/3KwDOeq
Download article (pdf) Citation Manager
Select type of program for download
| Endnote EndNote format (Mac & Win) | |
| Reference Manager Ris format (Win only) | |
| Procite Ris format (Win only) | |
| Medlars Format | |
| RefWorks Format RefWorks format (Mac & Win) | |
| BibTex Format BibTex format (Mac & Win) |
Article Publishing History
| Received: | 2023-02-21 |
|---|---|
| Accepted: | 2023-03-21 |
| Reviewed by: |
 Mohammad Tariq
Mohammad Tariq |
| Second Review by: |
 Abhay Agarwal
Abhay Agarwal |
| Final Approval by: | Dr Pradeep Koppolu |
Introduction
Candida is one of the most common microorganisms isolated from oral cavity in 30% of healthy individuals. (1) The most common form of candidiasis noted in practice by General Dentists is pseudomembranous candidiasis. This clinical scenario of medically compromised patient with other systemic conditions and presenting clinical lesions in oral cavity makes this case unique for discussion for general dentistry practitioners. Unlike pseudomembranous candidiasis which can be wiped with gauze, atypical presentation of candidiasis in hyperplastic form challenges a clinician to include it as a differential diagnosis. This variety of candidiasis is termed as chronic hyperplastic candidiasis and it has a characteristic hyperkeratotic plaque appearance resembling oral leukoplakia that cannot be wiped, and is usually asymptomatic seen on buccal mucosa and lateral border of tongue. (2) Due to its atypical appearance it is also named as candidal leukoplakia. It is known to be most commonly associated with smoking and smoking cessation could result in complete resolution. (3) Lesions could vary from small to large well circumscribed elevated white plaques and either have a nodular or speckled appearance. (4-9) According to some studies, this form of candidiasis is also known to progress to severe dysplasia and malignancy when compared to non-candidal leukoplakia. (10) However, other published articles expressed controversy on such malignant potential of these lesions. (2) Other oral conditions that have a similar appearance and to be included in differential diagnosis are leukoplakia, lichenplanus, pemphigoid/pemphigus and squamous cell carcinoma. (11)
Patient information
A 54-year-old female patient presented to our dental clinic for a problem focused exam with primary concern of white patches/ lesions in her mouth for last one week. Per patient’s history she was initially seen by her primary care physician for the same concern and was recommended to see a Dentist or an ENT specialist for further evaluation and management. During the consult and discussing patient’s medical history, patient disclosed that she has a medical history of severe eczema for which she is on multiple medications. Her medical records did not pull up any specific medications for eczema and the patient could not recollect names and dosage of her current medications. She stated that she takes Benadryl for symptomatic relief and to relieve itching from eczema. In regards to her history of presenting illness, the patient stated she had similar lesions a month ago which subside and flare up occasionally. Patient was seen by her primary care physician and was referred to a general dentist and an ENT specialist simultaneously. Patient did not give any symptoms of burning or pain in the history of presenting illness nor had any concerns during palpation. Patient’s unclear medical history and pharmacological management of other systemic conditions with atypical presenting lesions lead to challenges in the differential diagnosis and management.
Clinical findings
Clinical intraoral exam revealed multiple white eruptions disseminated over entire oral mucosa including all the soft tissue on buccal mucosa (Figure 1, 2, 3), tongue (Figure 4) floor of the mouth (Figure 5) and palate (hard and soft palate (Figure 6) with exception of gingiva. However, patient's history stated that occasionally such lesions were noticed on gingiva in the past. Lesions measured approximately 2-4mm in circumference. The lesions could not be wiped away with gauze, were not associated with pain and had a hard keratotic feel on palpation. No purulent, serous or mucus discharge was noted from the lesions. Presenting lesions had a combination of different varieties as mentioned in the presented clinical photographs. No other physical exam findings of lymph node involvement or signs of any systemic infection were recorded.
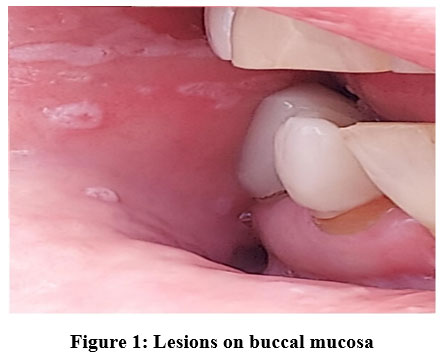 |
Figure 1: Lesions on buccal mucosa Click here to view Figure |
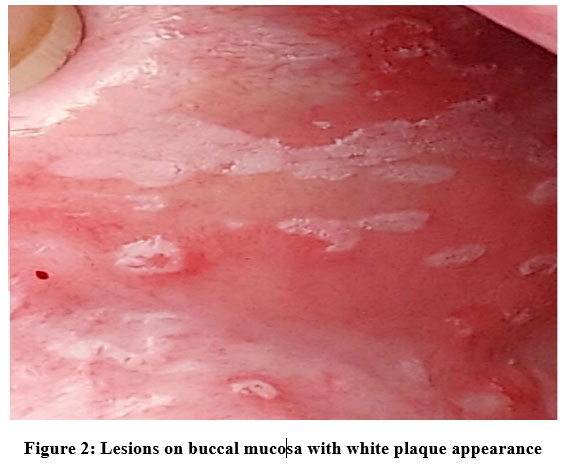 |
Figure 2: Lesions on buccal mucosa with white plaque appearance. Click here to view Figure |
 |
Figure 3: Lesions on buccal mucosa with lace like pattern Click here to view Figure |
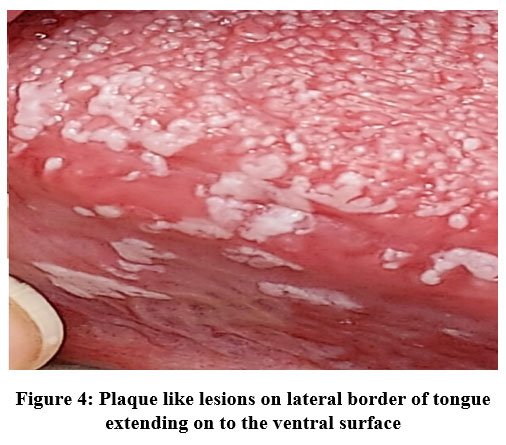 |
Figure 4: Plaque like lesions on lateral border of tongue extending on to the ventral surface. Click here to View Figure |
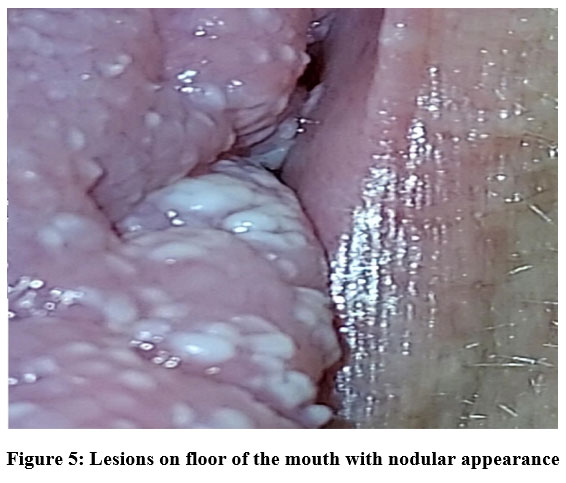 |
Figure 5: Lesions on floor of the mouth with nodular appearance. Click here to view Figure |
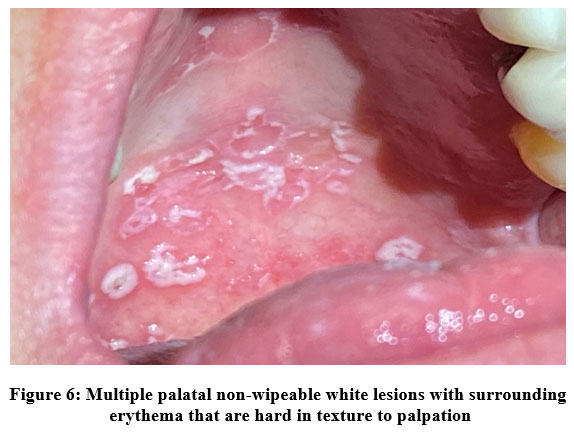 |
Figure 6: Multiple palatal non-wipeable white lesions with surrounding erythema that are hard in texture to palpation. |
Table 1: below is a brief description of presenting symptoms during patient’s appointments.
|
Appointment |
Presentation |
|
Initial presentation |
H/O lesions for One-week time period. Disseminated lesions over oral mucosa on palate, floor of the mouth and buccal/labial mucosa. No symptoms recorded. |
|
Follow up appointment |
3 weeks later, patient was followed up by ENT specialist and Primary Care Physician. Completely healed lesions with remnants of 2 small lesions in hard palate. |
Due to lack of diagnostic procedures at our facility, no diagnostic tools were used to arrive at a final diagnosis. This significantly contributed to the existing diagnostic challenges of unclear medical information from patient's history. Due to patient’s complex medical history and multiple unclear medications that patient is undergoing treatment for other systemic conditions, it was challenging to arrive at a final diagnosis without further tests. Few of the differential diagnosis that were considered included Hyperplastic candidiasis, Oral manifestations of eczema, leukoplakia, lichenplanus and oral pemphigoid/pemphigus. Due to lack of a final diagnosis, prognosis of treatment or resolving the clinical scenario remained unpredictable during the initial visit. However, as discussed below, a successful outcome of antifungal treatment that lead to almost complete resolution of lesions changed the prognosis of the presenting condition from unpredictable to excellent.
Therapeutic intervention, Follow up and outcomes
Due to lack of a final diagnosis, no therapeutic intervention was initiated in our practice. At a 3 week follow up appointment, as per patient's history, due to recent flare up of eczema, her primary care physician prescribed a very high bolus dose of steroid medications. Patient forgot to disclose this critical information during her initial visit in our practice. However, she disclosed this information during her visit to the ENT specialist and she was treated for yeast infection / thrush and that helped the lesions heal up. The ENT specialist made a professional decision to treat for hyperplastic candidiasis. Patient completed an entire course of Clotrimazole course prescribed by her ENT specialist. Patient brought in her prescription details of Clotrimazole. According to those records, ENT specialist prescribed Clotrimazole 10mg troche 5 times a day for 2 weeks. During the follow up visit, patient’s lesions healed up almost up to 98% with two small remnant lesions noted on the hard palate. Due to exceptional response of lesions to antifungal medications, a final diagnosis of hyperplastic candidiasis was derived.
Discussion
Limitation in this case report includes lack of diagnostic tests at our facility to attain a final diagnosis due to which the patient had to be referred out to an ENT specialist. Patient's unclear or partial disclosure of medical information in regards to her treatment for eczema posed a critical challenge in diagnosis, evaluation and management. When unsure and in a clinical dilemma with no access to further diagnostic tools, an unclear medical history and a challenging clinical lesion, referring to an ENT specialist can be considered as a strength in this case scenario. Though referral to an oral pathologist or an oral medicine department would be ideal, due to lack of such services in this specific geographical area, patient’s insurance and financial concerns dictated the patient to follow up with an ENT specialist. Though patient could not be treated at our facility, an arrangement of follow up with a concerned professional lead to patient's satisfactory experience and a successful outcome. Future collaborations with oral pathology department at UTHSC college of Dentistry through Tele Dentistry are being considered for handling similar patient scenarios.
Below is a brief discussion on variation in clinical presentation, contributing factors, diagnostic tests and pharmacological management for application in clinical dentistry
Table 2 discusses classification and clinical variation in presentation
Table 2: Classification and terminology.
|
Type/Variety/Presentation |
Features/Appearance |
|
Pseudomembranous candidiasis |
White plaque/curds. Most common form of candidiasis |
|
Acute atrophic candidiasis/ Candidal glossitis/Glossodynia |
Antibiotic sore mouth due to use of broad spectrum antibiotics. (12) |
|
Chronic atrophic candidiasis/ Denture stomatitis |
Erythematous lesion confined to oral mucosa in contact with denture surfaces. Usually due to poor denture hygiene. |
|
Angular chelitis/Perleche |
Usually associated with decreased vertical dimension in denture patients. Infection from combination of both staph aureus and candida albicans. (13, 14) |
|
Median rhomboid glossitis |
Rhomboid shaped lesion with atrophy of filiform papillae. (12) |
|
Chronic hyperplastic candidiasis/ Candidal leukoplakia |
White speckled/nodular appearance that cannot be wiped |
|
Candidiasis related to systemic conditions. |
Lesions could be one or more variations of the above |
Table 3 discusses local and systemic risk factors that contribute to develop candidiasis
Table 3: Contributing risk factors.
|
Local (15) |
Hyposalivation, Poor oral hygiene, removable prosthesis, local use of immunosuppressive topical, mucositis secondary to cancer therapy. |
|
Systemic (15-25) |
Immunosuppression from diseases (HIV/AIDS, Diabetes Chemotherapy or systemic immunosuppressant medications, nutritional disorders, endocrine disorders, radiation treatment, systemic corticosteroids, immunomodulatory drugs, polypharmacy leading to Hyposalivation etc. |
Diagnostic tests
10% KOH - Digests pseudo membrane and reveals spores, yeast forms and mycelia. (16)
PAS - Periodic Acid Schiff stain - A smear from infected area is fixed in alcohol and stained with PAS reveals fungal organisms under a microscope. (15,16)
Saboraud Agar plates - These can be used for culture to identify the causative organism and its species in cases where initial antifungal medications were not successful in treatment, immunocompromised patients and recurrence scenarios. (15)
Biopsy with fungal stain - This method can be used in clinical cases where chronic hyperplastic candidiasis did not respond to antifungal treatments and to rule out possible dysplasia or malignancy. (15) Table 4 below discusses medical management available for treatment.
Table 4: Treatment:*
|
Level of Treatment |
Criteria and Pharmacological agents |
|
Level 1 |
Mild oral infection with few underlying contributing factors
|
|
Level 2 |
Failed level 1 treatment or more systemic contributing factors. Combination of 2 agents from level 1 |
|
Level 3 |
|
|
Level 4 |
Severe clinical manifestations - Combination of level 2 and 3 could be utilized. |
* Adapted and modified from (4, 26)
Conclusion
Primary take away from this case report is to have a thorough knowledge of variation in presentation of oral candidiasis, differential diagnosis to be considered in atypical presenting lesions and ideal management or referral when clinically not possible to diagnose and manage in a general dentistry setting.
Acknowledgements
Thank you Ms. Mary Grace Hilario and Ms. Tonja Messer for helping with clinical photography.
Conflict of interest
The author(s) declare no conflict of interest.
References
- Cohen R, Roth FJ, Delgado E, Ahearn DG, Kalser MH. Fungal flora of the normal human small and large intestine. N Engl J Med. 1969 Mar 20;280(12):638-41. doi: 10.1056/NEJM196903202801204. PMID: 5764842.
CrossRef - Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia). Crit Rev Oral Biol Med. 2003;14(4):253-67. doi: 10.1177/154411130301400403. PMID: 12907694.
CrossRef - Silverman S Jr, Luangjarmekorn L, Greenspan D. Occurrence of oral Candida in irradiated head and neck cancer patients. J Oral Med. 1984 Oct-Dec;39(4):194-6. PMID: 6389802.
- Sharon V, Fazel N. Oral candidiasis and angular cheilitis. Dermatol Ther. 2010 May-Jun;23(3):230-42. doi: 10.1111/j.1529-8019.2010.01320.x. PMID: 20597942.
CrossRef - Farah CS, Ashman RB, Challacombe SJ. Oral candidosis. Clin Dermatol. 2000 Sep-Oct;18(5):553-62. doi: 10.1016/s0738-081x(00)00145-0. PMID: 11134850.
CrossRef - Ellepola AN, Samaranayake LP. Inhalational and topical steroids, and oral candidosis: a mini review. Oral Dis. 2001 Jul;7(4):211-6. PMID: 11575870.
CrossRef - McCullough MJ, Savage NW. Oral candidosis and the therapeutic use of antifungal agents in dentistry. Aust Dent J. 2005 Dec;50(4 Suppl 2):S36-9. doi: 10.1111/j.1834-7819.2005.tb00383.x. PMID: 16416716.
CrossRef - Farah CS, Lynch N, McCullough MJ. Oral fungal infections: an update for the general practitioner. Aust Dent J. 2010 Jun;55 Suppl 1:48-54. doi: 10.1111/j.1834-7819.2010.01198.x. PMID: 20553244.
CrossRef - Ellepola AN, Samaranayake LP. Oral candidal infections and antimycotics. Crit Rev Oral Biol Med. 2000;11(2):172-98. doi: 10.1177/10454411000110020301. PMID: 12002814.
CrossRef - Dreizen S. Oral candidiasis. Am J Med. 1984 Oct 30;77(4D):28-33. PMID: 6496525.
- Akpan A, Morgan R. Oral candidiasis. Postgrad Med J. 2002 Aug;78(922):455-9. doi: 10.1136/pmj.78.922.455. PMID: 12185216; PMCID: PMC1742467.
CrossRef - Millsop JW, Wang EA, Fazel N. Etiology, evaluation, and management of xerostomia. Clin Dermatol. 2017 Sep-Oct;35(5):468-476. doi: 10.1016/j.clindermatol.2017.06.010. Epub 2017 Jun 27. PMID: 28916028.
CrossRef - Akpan A, Morgan R. Oral candidiasis. Postgrad Med J. 2002 Aug;78(922):455-9. doi: 10.1136/pmj.78.922.455. PMID: 12185216; PMCID: PMC1742467.
CrossRef - Wilkieson C, Samaranayake LP, MacFarlane TW, Lamey PJ, MacKenzie D. Oral candidosis in the elderly in long term hospital care. J Oral Pathol Med. 1991 Jan;20(1):13-6. doi: 10.1111/j.1600-0714.1991.tb00880.x. PMID: 1900531.
CrossRef - Lalla RV, Patton LL, Dongari-Bagtzoglou A. Oral candidiasis: pathogenesis, clinical presentation, diagnosis and treatment strategies. J Calif Dent Assoc. 2013 Apr;41(4):263-8. PMID: 23705242.
CrossRef - Ray TL. Oral candidiasis. Dermatol Clin. 1987 Oct;5(4):651-62. PMID: 3315343.
CrossRef - Gonsalves WC, Chi AC, Neville BW. Common oral lesions: Part I. Superficial mucosal lesions. Am Fam Physician. 2007 Feb 15;75(4):501-7. PMID: 17323710.
- Fotos PG, Vincent SD, Hellstein JW. Oral candidosis. Clinical, historical, and therapeutic features of 100 cases. Oral Surg Oral Med Oral Pathol. 1992 Jul;74(1):41-9. doi: 10.1016/0030-4220(92)90213-a. PMID: 1508508.
CrossRef - Abu-Elteen KH, Abu-Alteen RM. The prevalence of Candida albicans populations in the mouths of complete denture wearers. New Microbiol. 1998 Jan;21(1):41-8. PMID: 9497928.
- Epstein JB, Gorsky M, Caldwell J. Fluconazole mouthrinses for oral candidiasis in postirradiation, transplant, and other patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002 Jun;93(6):671-5. doi: 10.1067/moe.2002.122728. PMID: 12142873.
CrossRef - Scully C. Drug effects on salivary glands: dry mouth. Oral Dis. 2003 Jul;9(4):165-76. doi: 10.1034/j.1601-0825.2003.03967.x. PMID: 12974516.
CrossRef - Farah CS, Ashman RB, Challacombe SJ. Oral candidosis. Clin Dermatol. 2000 Sep-Oct;18(5):553-62. doi: 10.1016/s0738-081x(00)00145-0. PMID: 11134850.
CrossRef - Ellepola AN, Samaranayake LP. Inhalational and topical steroids, and oral candidosis: a mini review. Oral Dis. 2001 Jul;7(4):211-6. PMID: 11575870.
CrossRef - Koba C, Koga C, Cho T, Kusukawa J. Determination of Candida species nestled in denture fissures. Biomed Rep. 2013 Jul;1(4):529-533. doi: 10.3892/br.2013.112. Epub 2013 May 22. PMID: 24648980; PMCID: PMC3917015.
CrossRef - Fangtham M, Magder LS, Petri MA. Oral candidiasis in systemic lupus erythematosus. Lupus. 2014 Jun;23(7):684-90. doi: 10.1177/0961203314525247. Epub 2014 Mar 5. PMID: 24598219.
CrossRef - Rhodus NL. Treatment of oral candidiasis. Northwest Dent. 2012 Mar-Apr;91(2):32-3. PMID: 22662470.
.jpg)




